Update from the Transition Unit - Friday 21 January 2022
Download a printable version of the newsletter:
Update from the Transition Unit - Friday 21 January 2022
[PDF, 1.2 MB]
Welcome to 2022
Nau mai ki te tau hou.
Kia ora and welcome to 2022 – a critical year that will lay the foundations for New Zealand’s future health system. As you all know, we have a large programme of work ahead of us before we transition over to the new system on 1 July.
While it’s exciting to look ahead at the transformational mahi to be done to deliver the reform programme, it is also important to pause and reflect on all that we achieved in 2021.
Some of our achievements include:
- Drafting and supporting the introduction of the Pae Ora (Healthy Futures) Bill - the legislation underpinning the reform
- Providing advice to Ministers on:
- Detailed system design including accountabilities for the core national entities and of sub-system operating models, like public health, localities and hauora Māori
- Future funding settings and investment priorities for the first few years of the new system
- Implementation and transition to the new system operating model
- How the Māori Health Authority can be accountable to Māori
- Future regulatory programme for workforce policy, and advice on workforce functions in the new system
- Establishing the two interim entities Health New Zealand and the Māori Health Authority, and supporting the appointment of Boards and interim Chief Executives to these entities, and supporting the Minister of Health to issue letters of expectation to the interim entities to provide direction for their establishment programmes
- Supporting a large number of hui regarding functions and powers of the Māori Health Authority, and the future role and responsibility of Iwi-Māori Partnership Boards
- Establishing workstreams to develop the interim New Zealand Health Plan and New Zealand Health Charter
- Supporting the design of a consumer voice framework that will help health entities to meaningfully engage with people using the health system
- Confirming the areas where the first locality prototypes are likely to be established
- Hosting a national roadshow with 20 dedicated hui to engage with the health workforce, and undertaking hundreds of engagements with people in the sector and wider stakeholders
- Transferring key workstreams from the Transition Unit to interim entities Health New Zealand and the Māori Health Authority.
Moving into 2022, our focus is firmly on ensuring we transition to the new health system with minimal disruption to the health workforce.
In the coming months, Health New Zealand and the Māori Health Authority will be undertaking further work on the New Zealand Health Plan – this will help determine ‘what’ the sector will do – and continuing our work to develop a Health Charter to establish a shared vision and culture across the sector, or ‘how’ the sector will work. Interim Health New Zealand and the interim Māori Health Authority will also confirm where we will prototype the localities approach to planning, commissioning and delivering health services.
At the Transition Unit, our role will be to continue producing policy and design advice on key features of the future system, and we will also provide ongoing advice to Ministers on how the new entities are progressing the Government’s reform agenda.
The Boards of the interim entities Health New Zealand and the Māori Health Authority are supporting the interim CEs and staff of each entity to secure the capacity and capability needed to develop their work plans and priorities ahead of 1 July.
On that note, I am delighted to again congratulate Fepulea’i Margie Apa and Riana Manuel on their appointments as the Chief Executives to lead Health New Zealand and the Māori Health Authority through their establishment phase and into the future. Both Margie and Riana will start in their new roles in mid-February.
Stephen McKernan, Director – Transition Unit
Margie Apa and Riana Manuel to lead health entities
The two Chief Executives to lead Health New Zealand and the Māori Health Authority were announced on 20 December.
Fepulea’i Margie Apa, currently Chief Executive of Counties Manukau District Health Board, has been appointed Chief Executive of interim Health New Zealand.

Margie Apa
Riana Manuel, currently Chief Executive of Hauraki Primary Health Organisation and iwi-based not-for-profit Te Korowai Hauora o Hauraki, has been appointed as Chief Executive of the interim Māori Health Authority.
Fepulea’i Margie Apa has more than 20 years of experience in health leadership and leads an organisation which provides health services to more than 600,000 people.
“To be part of a transformation that will, ultimately, improve people’s lives is a tremendous opportunity and I will work to ensure that change doesn’t distract us but enables us to do what we come to work for everyday – to improve health and wellbeing outcomes for all New Zealanders with a focus on achieving health equity for our most vulnerable,” Margie said.
Riana Manuel’s dedication to connecting and engaging with local communities was a key driver for her stepping up for the role.

Riana Manuel
“That is where you really see the impact of change,” Riana said.
“As a person who has been raised in my village (Manaia), I understand the need to effect change at a local level and am also aware of how local initiatives by Māori for Māori often have the biggest impact.”
Read the announcement about the new Chief Executives
Progress on second phase of localities
The Health Reform Transition Unit and interim entity Health New Zealand have begun planning for the second phase of localities.
A locality is a geographic area that makes sense to the people that live there. As a mechanism within the health system, it will support integrated care and enable services to be planned to address the needs of people within the locality. It’s a key feature of the future health system, ensuring a local approach to planning and delivering health services.
The first phase in the rollout involves establishing prototypes of the locality concept.
A long list of areas where prototypes may be established was confirmed in December
Helen Parker, Co-Director, Localities, said they were working with long-listed areas, and planning for the second phase.
“We’re taking a phased approach to introducing localities and we’re starting to look at areas that could be included in the second phase of the rollout. We’re expecting the second phase of localities to be confirmed in late 2022,” Helen said.
“We’re also developing the elements that need to be put in place in the background to support localities, such as a national collaboration to capture and share lessons as localities are rolled out.”
Helen said they are expecting proposals for the prototypes within the first phase to be submitted by 18 February, and would likely confirm the prototype areas in March or April.
“Over the next few weeks we will be checking in with these areas to discuss any further questions about the process for submitting a proposal to become a locality,” Helen said.
“We’re looking forward to seeing proposals that have been developed collaboratively with mana whenua partners, primary and community care providers and supported by District Health Boards.”
More information about localities
Reviewing the regulatory framework that supports our health system
Throughout New Zealand there are organisations that have a legal responsibility to help protect the health and safety of the public who are interacting with the wider health system.
These organisations, called ‘responsible authorities’, do this by making sure the people that provide healthcare have the necessary skills and experience to do their job.
We need to make sure the vision for a fairer, more equitable and consistent health system is supported by the work of these responsible authorities. That means making sure there is some oversight across any areas that might not align.
At the moment, Te Tiriti o Waitangi is not referenced in legislation that provides for responsible authorities. And the organisations involved in regulating people providing health services have tended to work in isolation, meaning opportunities to connect and collaborate have not always been realised.
The Health Reform Transition Unit and the Ministry of Health have been working together to take a look at how the arrangements for regulation align with the intended results from the health system reform.
Towards the end of 2021 we set up a number of online hui with organisations involved in this regulatory work to hear their thoughts and suggestions. About 30 organisations took part in the initial round of online hui, which has really helped develop our initial thinking.
We’ll be coming back to those involved in the regulation of healthcare workers over the next few months as we progress this opportunity to reset how people in Aotearoa New Zealand safely get the healthcare they need.
Shifting the system – providing a comprehensive range of support within communities
The vision for the future health system is one that is people-centred, equitable, accessible and cohesive.
To achieve that vision, the health system reform is focused on five key areas where we want to see significant change, referred to as 'system shifts'.
In this edition, we look at system shift two, how the future health system will provide people with the support they need, closer to home.
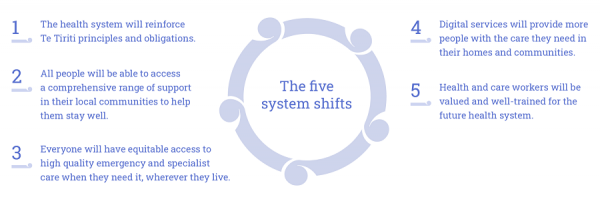
Within the future health system all people will be able to access a comprehensive range of support in their local communities to help them stay well.
It’s well understood that ensuring people get help for health-related needs sooner can prevent more serious issues in the long-term. This early access to care will be a key part of the new health system, with a greater range of local services available in all areas, designed around the holistic needs of communities.
All of these services will work together to improve population health – the term used to describe preventing illnesses and improving the health and wellbeing of local communities, considering all aspects of health, and other things that can affect people’s wellbeing like employment and housing.
People and whānau will be empowered to better manage their own health and wellbeing, and remain independent and connected through information, advice, community support and targeted services.
Health services will reach out into the community to support people at different stages of their lives. When people do need help, services will be provided in a way that suits what that person needs and prefers.
The localities concept is a key part of making this shift towards comprehensive care in the community. The idea is that different care and support providers will collaborate within a local area, working across sectors and organisations, to ensure people get the help they need to stay well – whether that’s a dedicated health service, or other social support.
