Update from the Transition Unit - Wednesday 17 November 2021
Kia ora
It has been another busy period for the Transition Unit as our work to reform the health system continues. A key priority has been on helping ensure the health workforce is aware of the changes to come, and has had the opportunity to learn more about areas of the reform that are relevant to them.
It’s been great to see so many people, from all parts of the health workforce, join us at various sessions as part of our national roadshow. Even where we’ve not always been able to see people in person due to COVID-19 alert levels, it’s been really encouraging that people have been able to make the time to listen to us – and we have really benefited from hearing from you.
We’re getting a great number of questions during these sessions. A good many we’ve been able to answer at the time, but I also want to acknowledge that some of the detail I know many of you are seeking we simply don’t have yet.
There is still a great deal of work to do in order to determine key elements of the new system, and in many cases, to reach that detail, we first need the sector’s help and input to inform aspects of the wider reform programme.
For example, the team working on the New Zealand Health Plan has established working groups to support its work, leveraging the valuable insights that those in the sector can bring. This type of engagement is happening across the board and, together, we will help to shape the detailed future of the health system in months leading up to 1 July 2022 when the new system comes into effect.
On that note, the legislation giving effect to the reforms is now working its way through Parliament’s select committee process. I encourage you to take a look at the Pae Ora Legislation select committee’s webpage(external link) and share your thoughts on the Bill – submissions close on 9 December.
With the interim entities officially established on 1 November, we are now supporting the boards of interim Health New Zealand and the interim Māori Health Authority on their work programmes. We look forward to providing an update on progress in future updates.
Finally, it’s important to note that COVID-19 continues to present unprecedented challenges for the health sector and we are mindful of people's capacity to engage with the health reform. Our focus remains on ensuring the new system comes into effect with as little disruption as possible to those working in the sector.
Stephen McKernan
Director – Transition Unit
Interim MHA Board to meet with Iwi Māori Partnership Boards
The interim Māori Health Authority will shortly carry out a further round of engagements to discuss and agree Iwi Māori Partnership Board powers and functions in the future health system. This series of virtual hui will take place through November and December and will include the current Māori Relationship Boards, iwi and hapū authorities, and Māori community and representative organisations.
“The Māori Health Authority will work with Māori communities, whānau, hapū and Iwi to establish the Iwi Māori Partnership Boards. The IMPBs will act for the communities they represent and bring the voice of whānau forward” says Tipa Mahuta, Co-Chair of the interim Māori Health Authority. It is envisaged that the core functions of Iwi Māori Partnership Boards to be considered will include:
- engaging with whānau and hapū, and sharing the resulting insights and perspectives with Health NZ, the Māori Health Authority, and the wider health system
- assessing and evaluating the current state of hauora Māori in their locality or localities, and to determine priorities for improving hauora Māori
- to agree locality priorities and plans with Health NZ and the Māori Health Authority
- monitoring the performance of the health system in their locality or localities, including against the locality plan
- reporting on their own activities to whānau and hāpori Māori, and other relevant partners.
“The Māori Health Authority and Iwi Māori Partnership Boards represent a new way of working to shape the future health system. Our collective challenge is to influence the new system in a way that sustains change, achieves equity of outcomes, and elevates the voice of whānau to be direction-setters not just service users” says Sharon Shea, Co-Chair of the interim Māori Health Authority board.
Following these virtual hui, the Minister of Health will report back to Cabinet with recommendations on how Iwi Māori Partnership Boards are ultimately reflected in legislation.
Work progressing to ensure longstanding inequity is addressed
The establishment of the interim agencies – the Māori Health Authority and Health New Zealand – and their immediate focus, signals progress is being made to address longstanding inequity in New Zealand’s health system, say their acting Chief Executives.
Acting Chief Executive of the interim Māori Health Authority, Chad Paraone, says achieving equity is a critical priority for the new entity, in line with the transformational objectives of the health system reform.
“The reform has been driven by the need to do things differently for members of the community that have been underserved by the system, and this is particularly the case for Māori,” Chad said.
“With the Māori Health Authority board appointed, and the Authority’s work programme for the next seven months underway, the plans we have around how we will address inequity are being progressed. Te Tiriti and equity are both front and centre of the reform programme.”
“As an immediate priority, the Authority is supporting the board to engage with the Māori sector to refine the scope and role of Iwi Māori Partnership Boards in the design and delivery of local health services,” Chad said.
“The Pae Ora (Healthy Futures) legislation will enable Iwi Māori Partnership Boards to play a significant role in the way health outcomes are delivered in the future – and equity will clearly feature strongly in that respect. A key focus for us is to engage with iwi and those boards to understand how they want to work together with the Māori Health Authority.”
Chad said the Authority’s ability to provide policy advice to the Minister, to directly commission kaupapa Māori services, to be part of Health New Zealand commissioning processes (co-commissioning), are all examples of how the new system has been designed to deliver on equity.
“A core role of the Authority will be to commission health services that are designed and delivered by Māori to better meet the needs of our local Māori communities. We’ve seen the real value of this in the recent Covid vaccination campaigns. We’ll be looking through a Māori lens to ensure that our communities get the support they need, when, where and how they need it. We’re currently focused on how that will work ahead of the entity formally coming into effect on 1 July 2022.
“We’ll also be working alongside Health New Zealand to both shape and support its work. This includes embedding equity in the planning and management of hospital and specialist services as well as in the commissioning of primary and community services. All areas of the health system must have a strong focus on delivering equity outcomes.”
“There is also a need to address the large, unwarranted differences in access and treatment that exist for many Kiwis based on geography, sometimes referred to as the ‘postcode lottery’. Having the variation in median waiting time and access thresholds which we have today, is unacceptable. Whānau in one part of the country should have largely the same (equal) access and waiting time as whānau elsewhere. That’s also important, alongside the central push for equity.”
Acting Chief Executive of interim Health New Zealand, Martin Hefford, said there were key areas the organisation was focusing on to kickstart progress on critical areas, and equity was a key priority.
“One of our first priorities is to develop an interim New Zealand Health Plan in partnership with the interim Māori Health Authority. This plan is designed to ensure the whole system is responsive to the needs of Māori and will set out how the system will achieve the five system shifts – one of which is to ensure the health system reinforces Te Tiriti principles and obligations,” Martin said.
“It will also set out early priorities to improve health outcomes and equity for Māori, Pacific, disabled people and other groups who experience poorer outcomes.”
“These early priorities sit alongside work to ensure our system is set up in a way that ensures improved healthcare access for everyone, regardless of where they live in New Zealand.”
There will be a range of engagement activities occurring across the motu early in 2022, including the NZ Health Plan and the NZ Health Charter. Look out for more information about engagement opportunities on the Future of health website.
Locality prototypes on track for early 2022
The Transition Unit is working with the interim agencies, Health New Zealand and the Māori Health Authority, to embark on a collaborative process to select locality prototypes that will become the first in the reformed health system.
Localities will enable a population health approach to drive locality planning and service delivery – integrating both health services and those that play a role in addressing the wider determinants of health.
The Transition Unit has been working to understand the barriers preventing this type of approach from being adopted throughout the sector. Some of the barriers that were identified include restrictive and inflexible contracting and funding models, a lack of integrated information systems hindering collaboration and relationships between funders, providers and communities.
The next steps involve selecting prototypes that will become exemplar models to inform a national roll out of localities - these are expected to be established by early March 2022.
Because this phase is about learning as much as possible, the Unit wants to get a good variety of geographic and community profiles across the prototypes. That’s why parameters have been developed to select the prototypes. These parameters were shared in a recent update and include areas with high Māori population, high Pacific population, high levels of deprivation and rural areas.
There will also be at least one prototype in each of the four regions within the future health system.
In addition to these objectives, the Unit wants to select areas where there is a high need for improvements to health outcomes, aligning with the intention to address inequity and inconsistency as soon as possible. The team is also developing the national infrastructure to support the prototypes and national roll out.
Over the next few months, the Transition Unit will be working with potential locality areas to refine what a prototype may look like. Confirmation of the prototype areas is expected in the first quarter of next year as the first tranche in a phased approach.
Shifting the system to improve the health of New Zealanders
The vision for the future health system is one that is people-centred, equitable, accessible and cohesive.
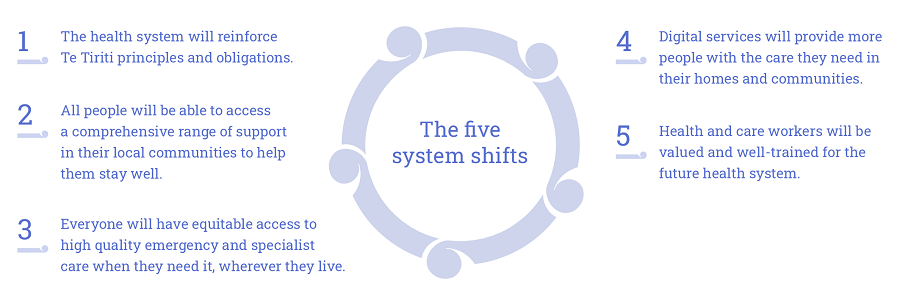
To achieve that vision, the Transition Unit is focused on five key areas that we want to see significant change, referred to as 'system shifts'.
These system shifts are future-focused, and describe the experience of people once the system is reformed.
The five key system shifts
- The health system will reinforce Te Tiriti principles and obligations
- Everyone will be able to access a comprehensive range of support in their local communities to help them stay well
- Everyone will have equitable access to high-quality emergency or specialist care when they need it
- Digital services will provide more people with the care they need in their homes and communities
- Health and care workers will be valued and well-trained for the future health system.
Over the next few editions we'll be taking a deep dive into these system shifts looking at what the Health and Disability System Review told us, a little bit more about how things will look in the future system, and the steps being taken to get there.
Future of health info sessions move north
The Transition Unit has been virtually visiting locations across the North Island this week following events across the South Island.
More than 1,000 people have joined the series of six events across the South Island over the last few weeks, gaining an overview of the reforms, the key initiatives underway, what’s coming up and how to stay informed about further opportunities to get involved.

Pacific health providers join the Dunedin roadshow
Deputy Director of the Health Transition Unit, Martin Hefford, said the South Island series had proven successful.
"[In the South Island] we had people attending either virtually or in-person from right across the health system. The people I talked to over a cuppa at the conclusion of the events all seemed to be very pleased they were able to attend, and appreciative that we had come to visit to provide an overview and update on the health reform and the progress being made," Martin said.
The roadshow has gone online and in-person this week for sessions throughout Bay of Plenty, Waikato and Hutt Valley ahead of Auckland on Friday.
“We had always hoped to be able to host all our information sessions in-person, rather than virtually,” Martin said.
“Unfortunately, COVID-19 alert levels have meant that isn’t possible in every location, so our North Island schedule is a mixture of in-person and entirely virtual sessions."
Registration links for further North Island events
“I really do encourage people to join if they can. South Island attendees I spoke to found it really informative and were pleased they participated. People in the health sector workforce are critical in delivering the health system transformation. It’s really important staff at all levels know what the reforms will deliver for them and for the people, whānau and communities they care for,” Martin said.
How to have your say on the Pae Ora (Healthy Futures) Bill
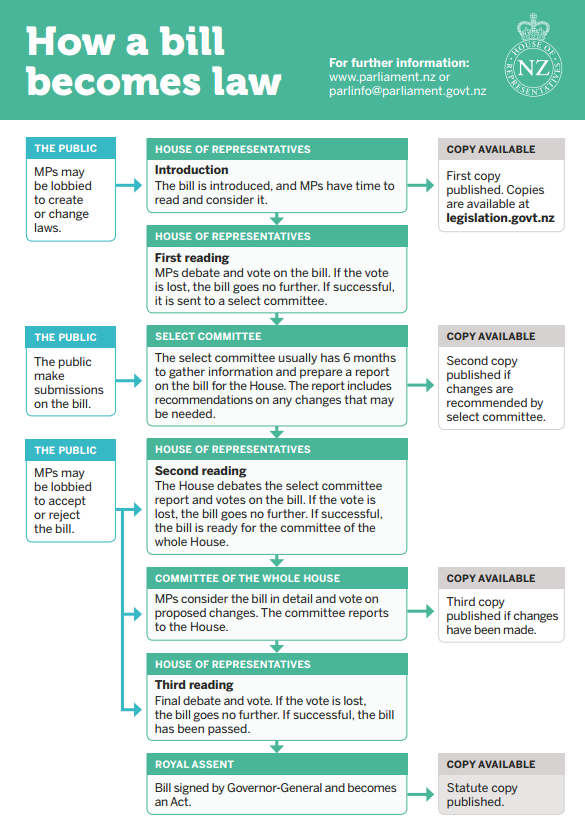
The Bill setting out the legislative framework for the future health system, the Pae Ora (Healthy Futures) Bill, is currently going through Parliament’s select committee process.
The bill provides for a new structure and accountability arrangements for the publicly-funded health system, in order to protect, promote, and improve the health of all New Zealanders.
Parliament has established a special select committee (the Pae Ora Legislation Committee) to consider the Bill. The special select committee has six months to consider the Bill before preparing a report for the House ahead of the second reading of the Bill.
The select committee has invited public submissions on the Bill. Submissions close 9 December.
- Find out how to make a submission(external link)
- Visit the Pae Ora Legislation Select Committee webpage(external link)
- Make a submission on the Bill(external link)
Recruitment underway for Public Health Agency
A new Public Health Agency will sit at the heart of the Ministry of Health, focusing on population and public health policy, strategy, regulatory, intelligence, surveillance and monitoring functions across the system. This will see more emphasis on the determinants of health such as employment and housing, which will mean working more closely with relevant government agencies and community partners.
Recruitment is now underway for the permanent Deputy Director-General of the Public Health Agency to lead the organisation and is expected to be complete in early 2022.
The Deputy Director-General of the Public Health Agency will report directly to the Director-General of Health.
Sector working groups support Health Plan development
The New Zealand Health Plan will be a foundational document setting out the fully costed plan for delivery of publicly-funded health services in the reformed system.
The Transition Unit has been working with the sector as it aims to develop an interim NZ Health Plan to be published in September.
Engagement across the sector has included setting up working groups to provide expertise and feedback in the key areas of the interim plan. These groups are focusing on integrated primary and community care, rural health, oranga kaumātua (healthy aging), mokopuna pae ora (early years), oranga hinengaro (mental health and addictions), national services and networks, planned care, and digital.
The Transition Unit’s next step is to engage with the wider sector to gather insights into examples of ‘evidence-based and developed practice’ that could be incorporated into the plan. Over the next few weeks we’ll let you know about opportunities to provide input.
People of the Transition Unit – Helen Parker
Helen Parker came to Aotearoa in 2013 for a short time...and never left.
She has joined the team helping to lead the development of the locality approach, leveraging off her 30-plus years of experience in health.

Helen Parker
Tell us a little about yourself
I’ve been fortunate to have three distinct but related careers in health, clinical, managerial and academic environments. This has given me exposure to how different countries and cultures approach health and health services. I qualified as a nurse in 1986 in the UK and spent some time in acute hospital care before taking a Specialist Practitioner degree in Community Health and District Nursing. I then moved into NHS community services commissioning and provider management roles. Completing a Masters degree in primary health care policy and management triggered my passion for how health systems work and develop. I have spent the last 15 years in consultancy, policy, academic and general practice ownership roles. I moved to Aotearoa late 2013 (just for two years!) and have worked at Pinnacle Midlands Health Network since then, now in my third year as CEO.
What’s your role as part of the health reform?
I’m on secondment to the Transition Unit as Co-Director, Localities which is great as it brings all my ‘careers’ into one role! The locality approach to improving health outcomes and addressing inequities is an opportunity for the sector to really think through what we know works...and what doesn’t…but also to transform and innovate in partnership with the Māori Health Authority, Iwi Māori Partnership Boards and other sectors that play a role in health outcomes.
I’m really enjoying working with Transition Unit colleagues and seeing how policy and reform intent can be shaped into something that makes sense to diverse communities and those who plan and deliver care.
What are you working on at the moment?
The Localities team is focused on getting the locality prototypes established early next year to test and refine the locality model to inform the national roll out. This includes recruiting a team to drive the locality approach, developing the framework for locality planning with Transition Unit colleagues and establishing an environment that will support lessons and insights to be gained from the locality prototypes.
We’re also planning the prototype evaluation which will be a critical component to development of the locality approach, capturing the impact on the intended system shifts and overall population health.
What happens next?
Top of our list is selecting the protype localities based on the agreed parameters and criteria. We will then be working to establish the supporting infrastructure to ensure they are successful.
What is your advice to the sector?
Those who have been through major system reforms before know it can be messy and uncomfortable for a while, especially for those who thrive on the detail. But if we keep focused on the ‘why’ we’ll ensure its not reform for reform’s sake. As a wiser person than me once said, it’s hard to put people, whānau or communities at the centre if you are standing there yourself. As health professionals we’ll need also to shift to see the change we want to see.
Printable version
Update from the Transition Unit - Wednesday 17 November 2021 [PDF, 2.2 MB]
